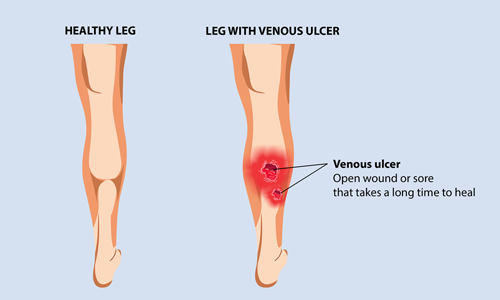
Venous Leg Ulcer
Annually, more than 1 million* people in India are diagnosed with a venous leg ulcer.
Venous leg ulcers, also known as stasis ulcers, are open wounds or sores that are chronic in nature (long-lasting). They can take months heal. If left unattended, these wounds increase in size with time. Venous leg ulcers occur on the skin of the lower leg (below the knee) and are commonly located just above the ankle, on the inner leg. Venous ulcers look like bleeding patches of skin with unevenly shaped borders and may or may not be painful. Venous leg ulcers are the most common types of leg ulcers.
Don’t confuse venous ulcers with diabetic foot ulcers and arterial ulcers. Diabetic foot ulcers are a serious complication of diabetes and are caused due to altered or complete loss of sensation in the leg (also known as peripheral neuropathy). Diabetic foot ulcers look like exposed flesh on the feet, surrounded by a border of thickened, coarse skin.
Arterial ulcers, on the other hand, develop because of damage to the arteries due to lack of blood flow to tissues. Arterial ulcers are usually located on the lateral surface of the ankle and they resemble an open sore that is often red, yellow, or black in colour.
Venous leg ulcers occur when you have damaged or inefficient veins. A person suffering from chronic venous insufficiency has poor blood circulation and weak vein walls that are stretched out. This causes the blood to pool in the legs and feet. The tremendous pressure increase in the veins, makes these people more prone to cuts and wounds. Even a minor injury can turn into a venous leg ulcer. The poor circulation makes these very difficult to heal.
The following complications increase the risk of developing venous leg ulcer:
- Obesity increases the pressure on the veins in the legs
- Blood clotting as a result of deep vein thrombosis increases the chances of developing venous ulcers
- Enlarged and inefficient varicose veins severely affect the vein valves, making those affected prone to developing venous ulcers
- Surgeries or previous injuries make it difficult to walk and tense the calf muscles, thus affecting blood circulation
- People over the age of 60 and women have higher chances of developing a venous ulcer
- Smoking interferes with the normal blood circulation and causes sores on the skin
- Past history of the condition in the family increases its diagnosis
- Pregnancy increases the pressure on the veins of the legs, thus increasing the chance of developing venous disorders
- Blockage of lymph vessels causes fluid build up in the legs, thus affecting blood circulation
Venous leg ulcer symptoms are overtly visible, which include:
- Swelling, aching, heaviness, and tiredness in legs
- Discolored, darkened, hardened skin around the ulcer
- Red, flaky, and itchy skin on the legs
- A foul-smelling discharge from the wound
- Formation of pus and onset of fever indicating an infection
- Stasis dermatitis indicating venous insufficiency
- Warm or hot skin with unevenly shaped borders
- Shallow sore with a red base
- Blockage of lymph vessels causes fluid build up in the legs, thus affecting blood circulation
Treating a venous leg ulcer can take months, depending on the size and other complications. With appropriate care, infection can be controlled, and the healing process can be accelerated.
In most cases, debridement is necessary. Debridement is the cleaning of the wound and removal of dead tissues and any other foreign particles. This is an important step in treating venous ulcers as it lays the basis for the healthy healing of the sore.
Once the wound has been cleaned thoroughly, wear firmly fitting compression socks/stockings on the leg. These socks aid healthy blood circulation by squeezing the veins. Using compression therapy is a proven method of treating venous leg ulcers as it prevents the pooling of blood in the legs and treats leg pain and swelling.
Adopting a healthy lifestyle is an easy way of avoiding the risks of a venous ulcer. Simple yet effective steps like the ones mentioned below go a long way in steering clear of the venous disorder:
- Quit smoking
- Avoid sitting or standing for long hours
- Exercise regularly
- Follow a healthy diet
- Elevate your legs at a certain angle
- Wear compression stockings for improving blood circulation
- If on medication, avoid skipping doses
- Maintain a normal BMI
If you are facing any of the above symptoms, meeting a doctor will certainly help.Get in touch with an expert and manage the symptoms of venous ulcers effectively.
*Source: Apollo Hospitals




